The nervous system of the gut (the enteric nervous system or ENS) plays a pivotal role in the functioning of the gastrointestinal tract, regulating digestion, absorption, and even influencing immune responses. Often referred to as the "second brain," the ENS contains a complex network of neurons that operate independently from the central nervous system but communicate with it extensively. This intricate system not only controls the routine functions of the digestive system but also communicates bidirectionally with the brain, impacting emotions, mood and even cognitive functions. This gut-brain connection involves complex pathways of nerves, hormones and transmitters which have been shown to be profoundly impacted by the gut microbiome. Understanding the importance of the enteric nervous system, and the role of the gut microbiome, sheds light on the profound connection between gut health and overall well-being, highlighting its significance in both physical and mental health. To learn more about the basics of the gut microbiome, read our article Microbiome 101: A Guide To Your Gut Microbiome.
The gut microbiome, consisting of trillions of microorganisms residing in your digestive tract, is primarily established early in life. During birth, a baby's gut is initially colonized by microorganisms from the mother's birth canal or skin, and later, through breastfeeding, which provides beneficial bacteria.
Each person's gut microbiome is influenced by genetics, lifestyle, diet and environmental factors. This complex ecosystem of bacteria, fungi and viruses not only aids in digestion but also impacts various aspects of health, from immune function to mental well-being. The origins of your gut microbiome are deeply intertwined with your life experiences, starting from the moment you enter the world.
The association of certain configurations of the gut microbiome with mental health conditions such as depression, anxiety, bipolar disorder and schizophrenia underscores the importance of the gut-brain axis. Changes in gut microbial composition can affect mood regulation and neurotransmitter production, influencing mental well-being.
Research suggests a link between the gut microbiome and several mental and psychological conditions. The connection between the gut microbiome and Autism Spectrum Disorder (ASD), highlights the microbiome’s role in neurodevelopment. Furthermore, other mental disorders such as anorexia nervosa, PTSD and ADHD are also linked with complex changes in the gut microbiota, demonstrating the importance of understanding and addressing gut health for overall mental well-being. The specific relationships between changes in the gut microbiota and mental disorders are shown in the figure linked here.
Specific gut bacteria have been associated with depressive symptoms in various Studies. Differences in gut microbiota composition, including reductions in alpha diversity and specific bacterial families, have been observed between healthy individuals and those with Major depressive disorder (MDD). These are associations and do not necessarily indicate causation.
Certain butyrate producing bacteria, like Dialister and Coprococcus spp., have been shown to be decreased in patients with depression, which may be due to the potential neurotransmitter effect of butyrate. However these studies did not adjust for confounders including lifestyle factors and medication use, which are known to modify the gut microbiome. Alternatively, other bacteria, such as Prevotella, Klebsiella, Streptococcus, and Clostridium XI, have been shown to be elevated in depressed patients.
Overall, these findings suggest that targeting gut microbiota could offer potential avenues for the prevention and management of depression. It’s important to note that not all cases of depression are linked with the gut microbiome. The only way to know if your gut microbiome shows patterns associated with depression is to test and analyze your own microbiome.
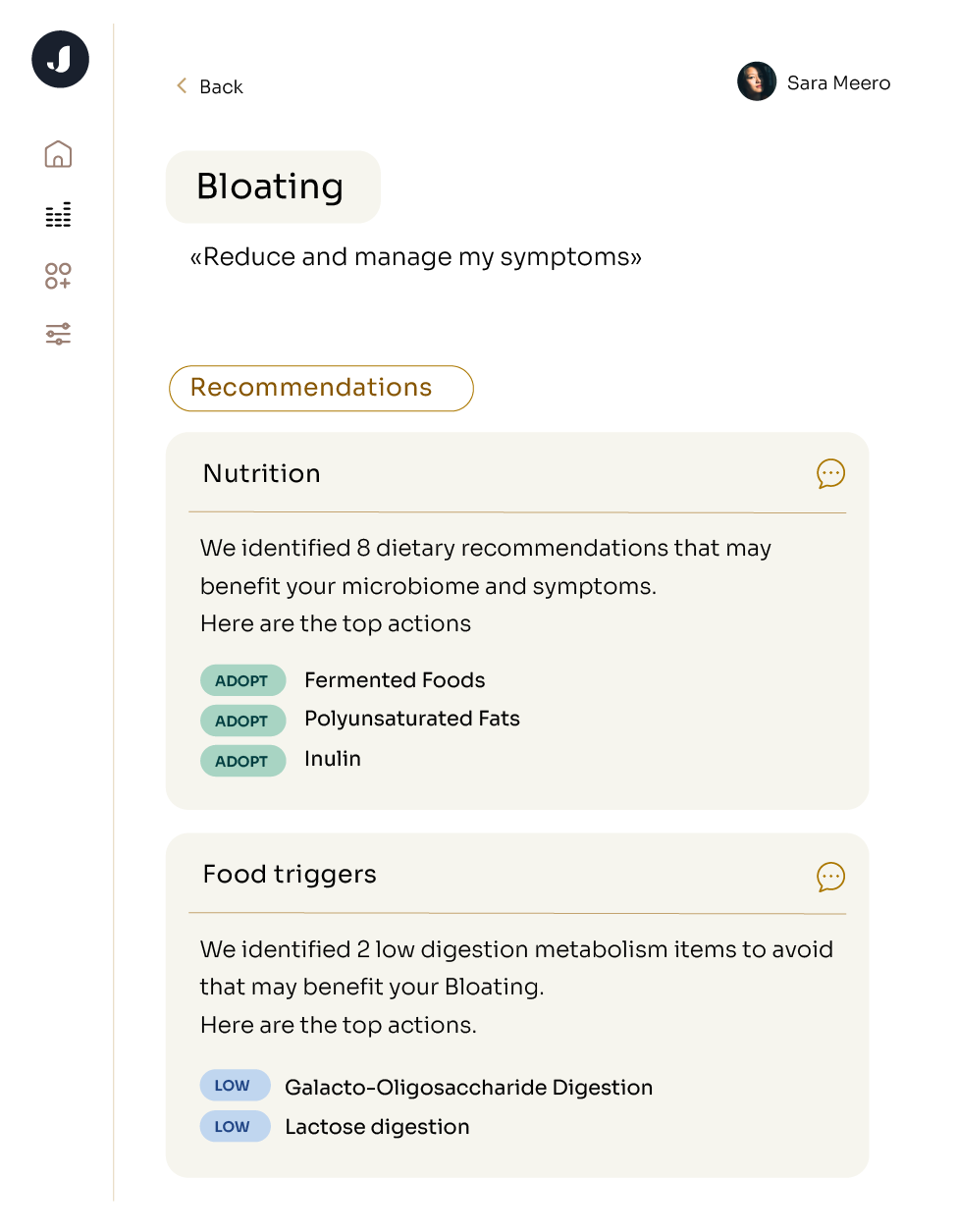
Improving mental health often involves nurturing a healthy microbiome, as highlighted in the article How to Improve the Gut Microbiome. One key strategy is to adapt your diet to include gut microbiome-friendly foods while also incorporating probiotics and prebiotics, which can play crucial roles in supporting mental well-being. Additionally, managing stress through practices like meditation, yoga, or deep breathing exercises is vital, as stress can significantly impact the gut-brain axis and contribute to mental health challenges. Prioritizing adequate sleep and regular exercise, as discussed in The Link Between Exercise and the Gut Microbiome, is also essential. These lifestyle adjustments can foster a resilient microbiome and contribute to a healthier, more balanced mental state. Although these strategies generally apply to maintaining a healthy microbiome, it’s important to emphasize that everybody’s microbiome is different and personalized testing and analysis is the only way to know what’s going on in your microbiome or how to personalize actions to change your microbiome to achieve your health goals.
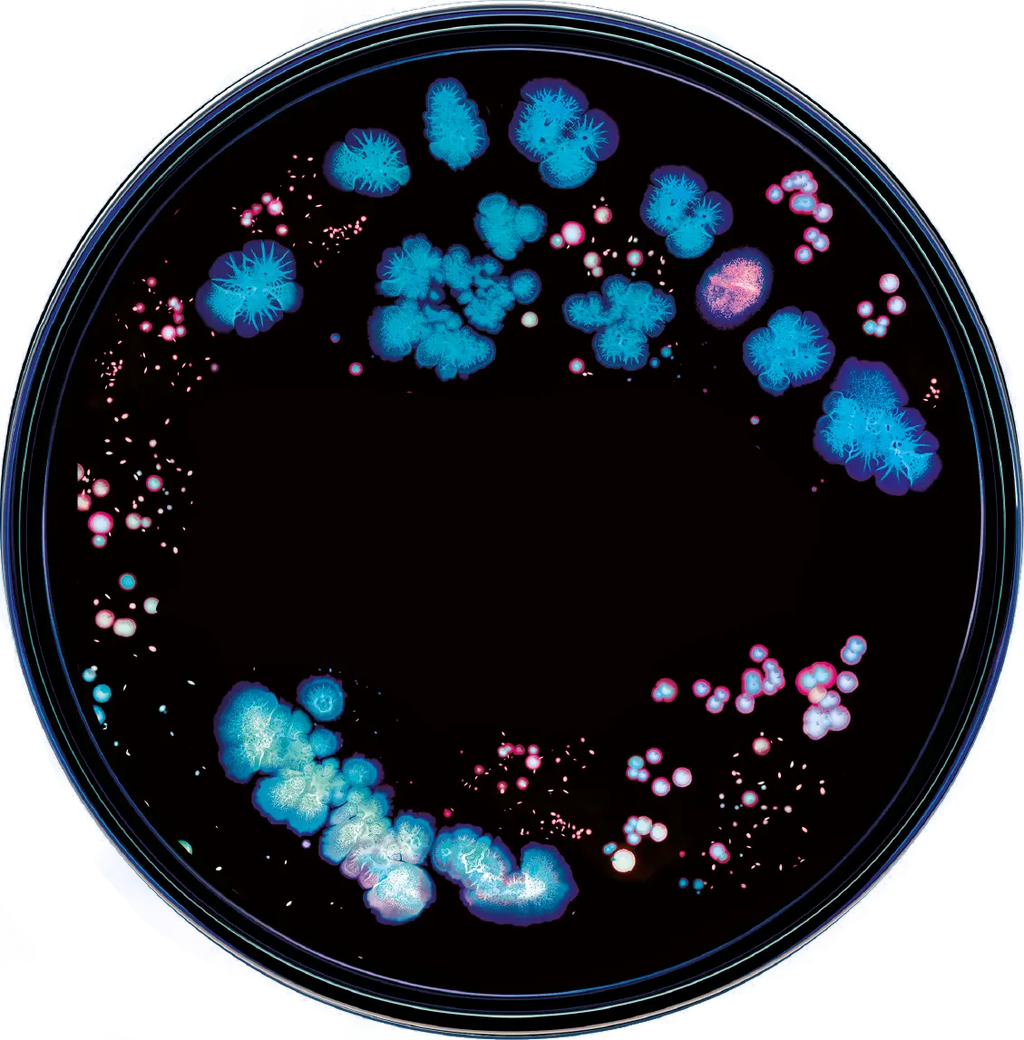
Understanding the composition of the microbiome is critical to understanding the intricacies of the mind and body, as it provides insight into the abundance or deficiency of specific bacteria within.
Research suggests that the gut microbiota plays a significant role in the communication between the brain and gut in both directions, influencing the production of neurotransmitters and hormones critical to mental well-being. Through dietary interventions, individuals can selectively increase or decrease the populations of specific bacteria known to positively or negatively impact mental health (Carabotti et al., 2015).
For example, increasing the consumption of fiber-rich foods can promote the growth of certain bacteria, such as Bifidobacteria and Lactobacilli, which are associated with improved mood and cognitive function (Fu et al., 2022). More specific interactions between dietary choices and organisms linked to mental health are shown in this figure, underscoring the significant role diet plays in shaping the composition of the microbiome and subsequently influencing mental health. As above, your own personal specific microbiome (as assessed through testing) will determine the associations for mental health and the specific dietary choices you can make to improve your microbiome.
Probiotics, as live microorganisms conferring health benefits, and prebiotics, as non-digestible fibers nourishing beneficial gut bacteria, may modulate gut health and influence hormonal balance. Although, the precise mechanisms linking gut health, hormones and mood are still under investigation. While there is some promising research suggesting that probiotics and prebiotics may enhance serotonin production, a neurotransmitter associated with mood regulation, through their effects on gut bacteria, there is some controversy. Definitive evidence from randomized controlled trials linking probiotics, prebiotics, and mood improvement is not yet available. To learn more, visit our other blog posts about probiotics, how to shop for them, and the controversy of their use.