Introduction
Major depressive disorder (MDD), commonly known as depression, is a mental health condition affecting millions of individuals worldwide, affecting approximately one in six adults in their lifetime. MDD can manifest as feelings of sadness, hopelessness, and worthlessness, often interfering with an individual’s daily life. Both heritable and environmental factors are believed to be involved in the development of the disease, however, there is no single established mechanism to comprehend depression in full.
In recent years, an intricate relationship has been revealed between our gut and health: both physical and mental. Emerging research suggests that the trillions of organisms in our gut may play a pivotal role in the development and progression of MDD. The microbiome not only plays a critical role in digestion, immunity, and metabolism, but also in regulating brain function and behavior. This relationship is likely bidirectional - Just as the microbiome can influence brain function and behavior, the brain, through various mechanisms, may also affect the composition and activity of the gut microbiota. This bidirectional communication underscores the complexity and significance of the gut-brain axis in the context of MDD.
The Gut-Brain Axis
The gut-brain axis is a bidirectional communication system that links the central nervous system (CNS), made up of our brain and spinal cord, and the enteric nervous system (ENS) in the gastrointestinal (GI) tract. In fact, the GI tract is often referred to as our “second brain.” This connection allows for constant communication between the gut and the brain through a number of neural, immune and hormonal signals so that changes in our gut can influence our brain and vice versa.
While certain phyla, such as Firmicutes and Bacteroides, are prevalent and collectively account for three-quarters of the microbiome in healthy individuals, the specific composition and quantity of microbes can vary widely from person to person. This diversity underscores the complex and personalized nature of the gut microbiota, challenging the notion of a uniform microbial landscape even among healthy people.
The Gut Microbiome and MDD
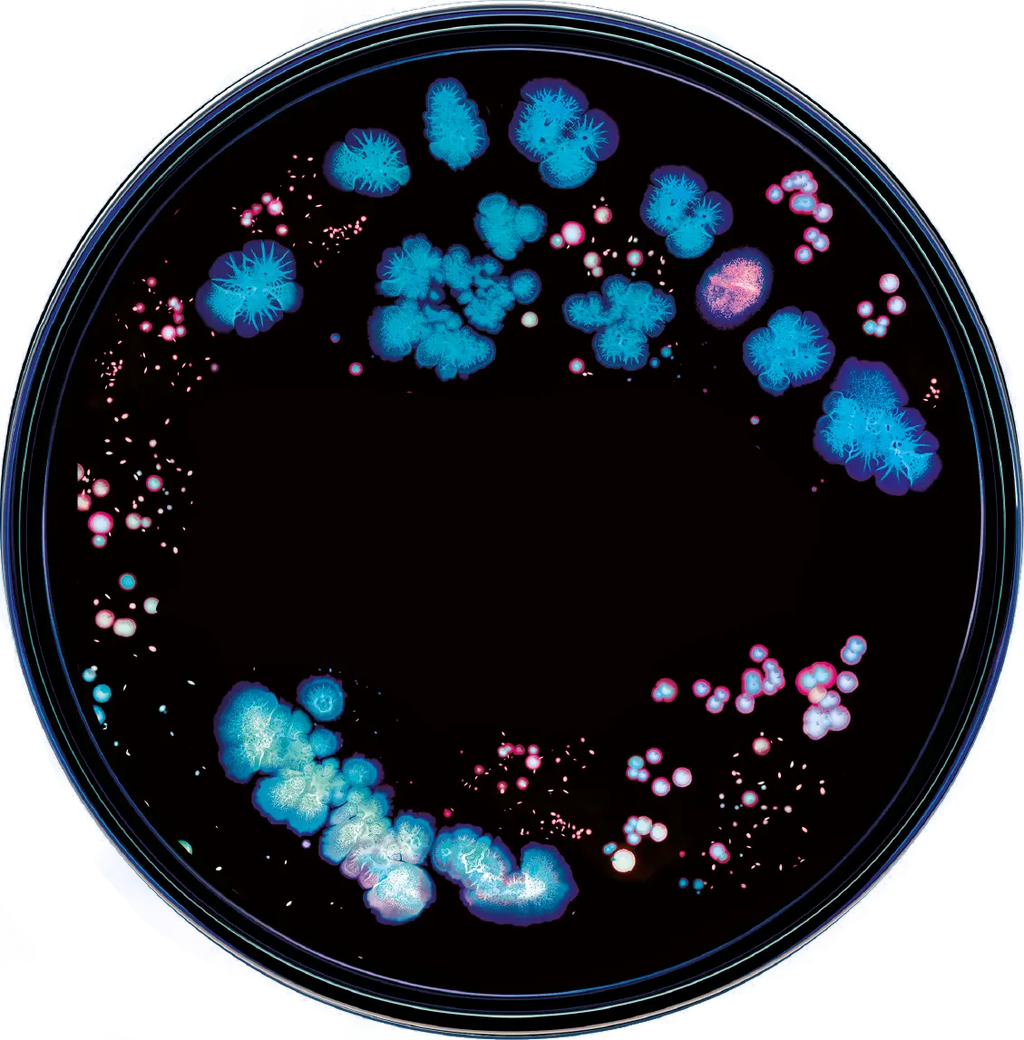
In the case of MDD, studies have shown that depressed individuals have a different gut microbiome compared to individuals without depression. For example, a study in Nature has linked thirteen microbial taxa with depressive symptoms. Additionally, the biodiversity of the microbiome has been associated with the degree of symptom severity.
The Firmicutes to Bacteroidetes ratio has been suggested as a potential biomarker for depressive symptoms, as it has been shown that there is a substantial decrease in Firmicutes in individuals with MDD in relation to healthy controls.
We are still understanding the exact role of the microbiome with depression. However, these are some pathways in which the gut microbiome has been suggested to be linked to major depressive disorder:
Neurotransmitter Production
Neurotransmitters are the messengers in our brains and play a key role in regulating mood and emotions. There is growing evidence that gut bacteria are involved in the metabolism of neurotransmitters; while the majority of serotonin is produced by human cells, gut bacteria can modulate the rate of production, influence the bioavailability of serotonin precursors such as tryptophan metabolites, and may even produce neurotransmitters themselves. In fact, over 90% of our body’s serotonin is secreted into our gut by intestinal enterochromaffin cells. Escherichia and Enterococcus have been revealed to be producers of serotonin. Additionally some strains of Bifidobacterium and Lactobacillus have been shown to be producers of gamma-aminobutyric acid (GABA), our main inhibitory neurotransmitter.
Inflammation
Chronic inflammation is associated with certain gut microbiome compositions. Inflammation has additionally been linked to various mental health disorders, including depression. Proinflammatory bacteria like Eggerthella and Atopobium have been expressed in higher relative abundance in individuals with MDD in comparison to healthy controls.
Stress Response
The body’s stress response system can be influenced through the gut-brain axis. Chronic stress is a known risk factor for depression, and an imbalanced gut microbiome may exacerbate stress-related symptoms. Stress has been linked to a “leaky gut”, where the gut barrier’s permeability increases, allowing harmful bacteria to seep in. Dietary fiber and fats have been suggested to alter the gut microbiome and therefore influencing production of short-chain fatty acids and lipopolysaccharides, which are possible triggers for a leaky gut. Research on human models is still underway.
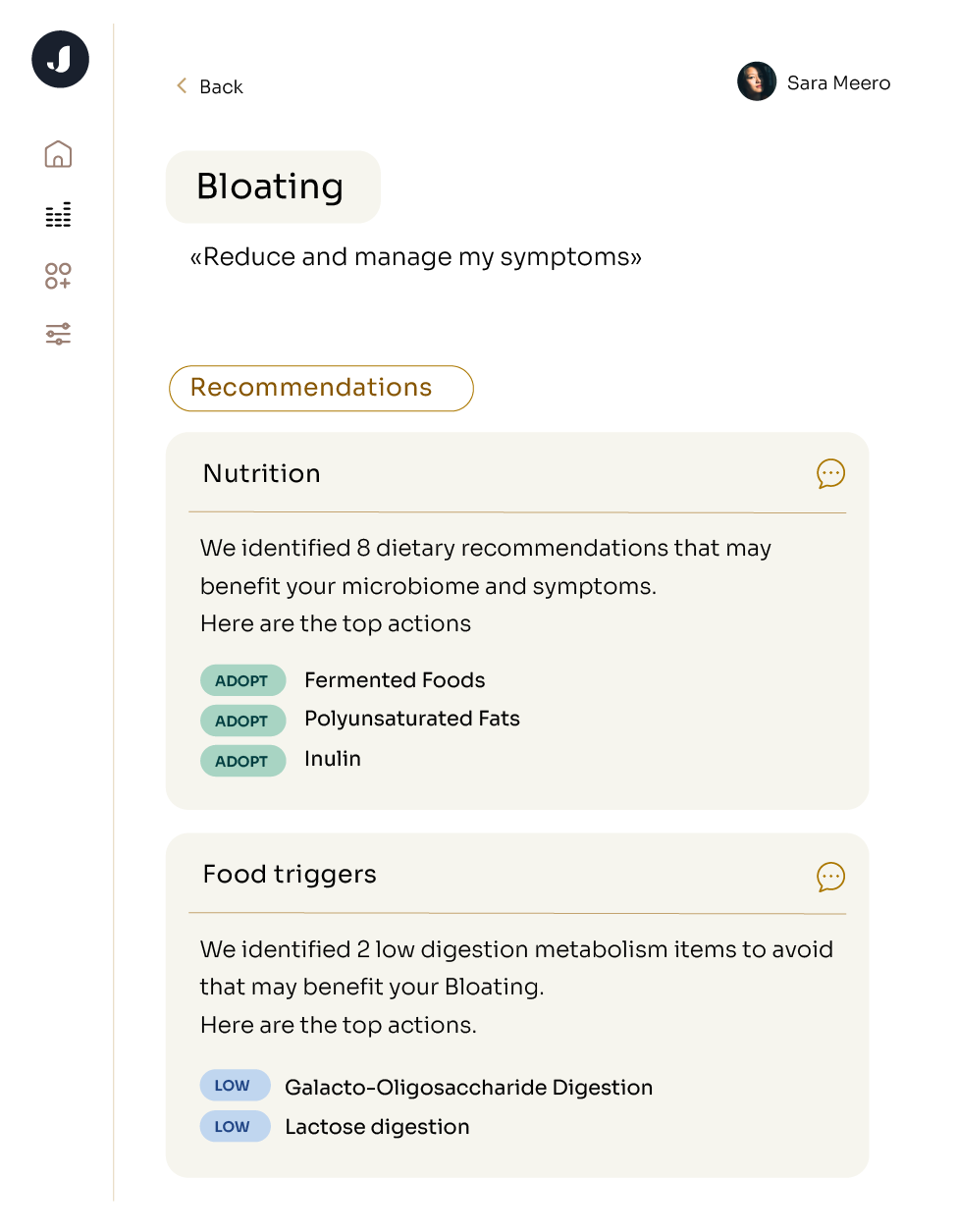
Analyzing your microbiome with a service such as Jona can allow you to identify any elements of your microbiome associated with depression or any of these pathways, and provide concrete actions that can help you change your microbiome.
Future directions for treatments
Traditionally, MDD has been treated with antidepressants and psychotherapy, but currently the gut microbiome is being explored as a new avenue in the search for an effective treatment due to its potential. Antidepressants are the current standard for treatment; however, they do not work in all people with MDD, with around 10-30% being classified as non-responders to treatments. While the link between the gut microbiome and MDD is still a subject of ongoing research, several studies have provided intriguing insights. This is a promising avenue for potential therapeutic interventions. Here are the treatment pathways we believe further microbiome knowledge can unlock:
Personalized Medicine
Consider the potential for treatments as unique as your microbiome. While the idea of personalized treatments based on an individual's gut microbiome profile is intriguing, it's essential to acknowledge that the evidence supporting this concept is still evolving, and there are conflicting findings in the scientific community. Research is ongoing, and as we delve deeper into the complexities of the gut-brain connection, the promise of tailored treatments remains an area of active investigation.Nutritional interventions could be complementary to current traditional therapies.
Nutritional Psychiatry
The role of diet in shaping the gut microbiome and its impact on mental health is an exciting area of exploration. Current psychiatric treatments may have side effects, and substituting or complementing these treatments with nutritional approaches could help mitigate the side effects.
Research has suggested that certain probiotics may improve depression-related symptoms in some people. However, the efficacy of probiotics for MDD treatment is still controversial, with contradicting evidence blurring the picture. The antidepressant qualities of probiotics and the efficacy of probiotics on the general population are currently still under research.
Microbiome-based Therapies
Developing microbiome-based therapies, such as precision probiotics or microbial transplantation could offer new ways to address MDD and related mental health conditions.
The two first patients with MDD ever treated with microbiome transplantation both showed improved depressive symptoms after transplantations. Although additional rigorous clinical trials evaluating the use of microbiome transplantation are needed, the modification of the microbiome via microbial transplants is an exciting area of treatment for MDD.