Irritable bowel syndrome (IBS), a type of functional gastrointestinal disorder (FGID), is a common condition that can have a significant impact on your quality of life. While the exact pathogenesis of IBS is not fully understood, genetics, diet and lifestyle, and alterations in the gut microbiome are all thought to have an affect on its development. A condition like this can cause significant discomfort that may prevent you from participating in activities. It is possible that severe symptoms of IBS may also affect one’s ability to work. This raises the question: is IBS a disability? In this article we will explore this question while shedding light on the implications of living with and managing IBS.
IBS flare-ups describe a period of time where individuals experience increased intensity of frequency of primary symptoms localized to the abdominal area or gastro-intestinal system. The duration of flare-ups, also called attacks, can vary greatly from individual to individual with several factors including symptom severity, IBS subtype, and management strategy potentially having an influence on how long the flare-up will last. On average flare-ups can last anywhere from a few hours to a few weeks.
Several studies have found a high incidence of psychological symptoms such as stress and anxiety in IBS patients, but what is the mechanism behind this phenomenon? The gut-brain axis may hold the answer. IBS can reduce your quality of life,, and this decrease can subsequently cause negative emotions such as embarrassment, anxiety, and depression. But, there is potentially a deeper link between the emotional and gatro-intestinal symptoms of IBS through bi-driectional communication between the gut and brain. This communication, often involving the gut microbiome, is thought to have effects on visceral sensitivity, immune and inflammatory response, and many other processes related to IBS. While research into the gut-brain axis is still in its infancy, this pathway offers a promising explanation of the comorbidity of IBS and psychological and emotional symptoms and conditions.
IBS has been linked by research to changes in the microbiome. It has been found that individuals with IBS of all types have decreased levels of some beneficial fermenting bacteria like Bifidobacterium and Faecalibacterium. These bacteria are important fermenters of complex carbohydrates including soluble fibers. Through the fermentation process, they produce short-chain fatty acids (SCFAs). Low levels of SCFAs could potentially contribute to IBS symptoms as they are responsible for controlling inflammation and maintaining intestinal barrier integrity. Other potential pathogenic bacteria such as Escherichia/Shigella were found to be increased in IBS patients. Although some patterns are seen across all IBS subtypes, there are unique microbiome signatures seen in each. See our blog post all about IBS and flare-ups to learn more about the microbiome signatures of IBS.
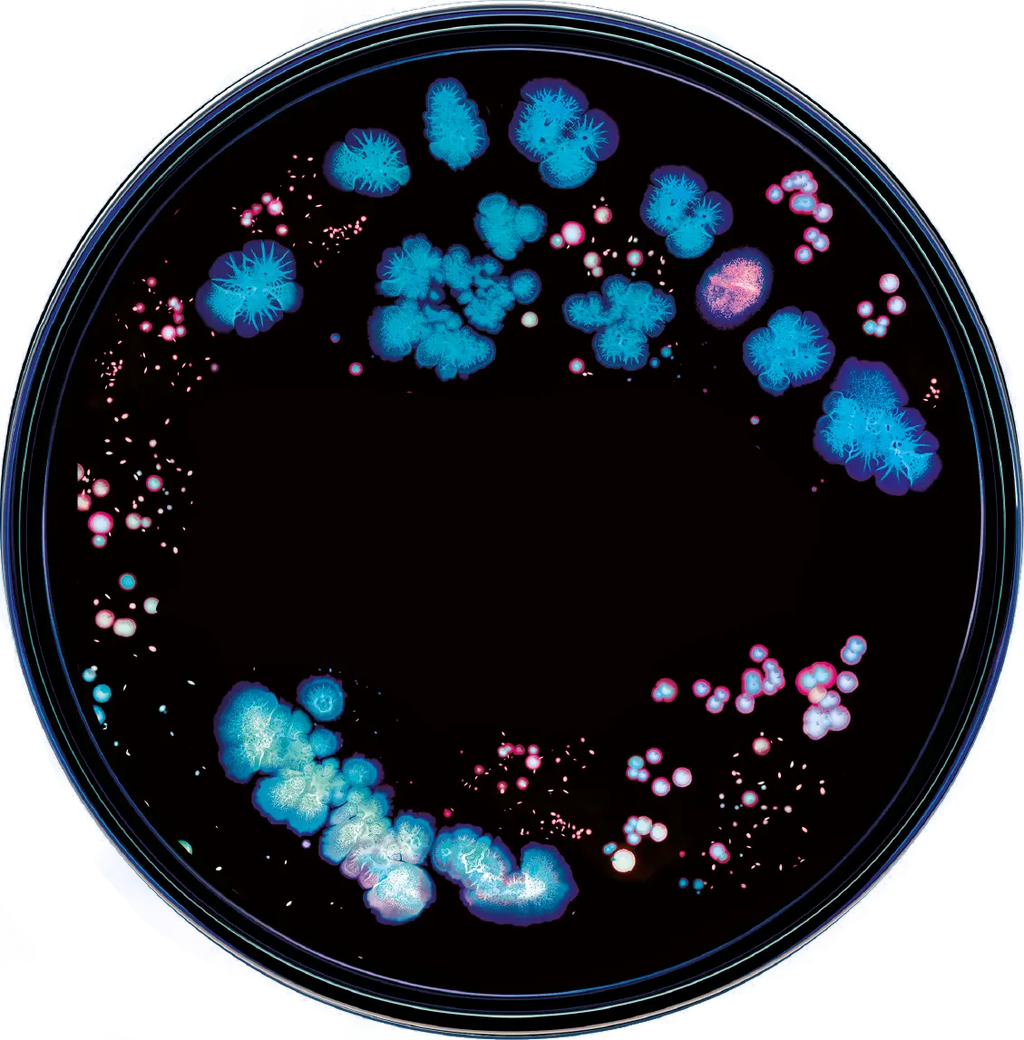
Oftentimes the word diversity comes up when considering the health of an individual's microbiome, but what is diversity? Diversity is a term used to describe the variety of organisms living in a particular ecosystem, in this case, the ecosystem is your gut. Diversity can be calculated in many ways, but it is typically either species richness (the number of different organisms you have in your gut), species evenness (the relative abundance of those organisms) or a combination of both. It is considered generally good to have a high diversity of organisms in your gut for multiple reasons. One major reason is high diversity usually comes with high redundancy, meaning multiple microbes in your gut can carry out the same function. This way, if one group of microbes is unable to carry out their function, there is another group to carry the slack. A diverse and redundant microbiome can increase the stability of your microbiome and make it more resilient and resistant to harmful disruptions.
Manage Stress
The best way to avoid experiencing an IBS flare-up is avoiding triggers. As detailed earlier, it is possible that stress and anxiety can trigger symptoms of IBS. Some helpful management strategies include gentle stretching, meditation, and yoga. These activities can relax your mind and body, resulting in reduced severity or frequency of symptoms.
Exercise Regularly
Some studies have linked moderate exercise to improved IBS symptoms or that individuals who regularly engage in physical activity are less likely to experience worsening symptoms than those that do not exercise. Use caution when changing your exercise practices, as intense physical activity can sometimes trigger IBS symptoms.
Stay Hydrated
Making sure you are hydrated is vital to managing symptoms of IBS. Water is a critical element in the functioning of your body, including your digestive tract. Dehydration can lead to changes in gut motility as well as other unfavorable symptoms.
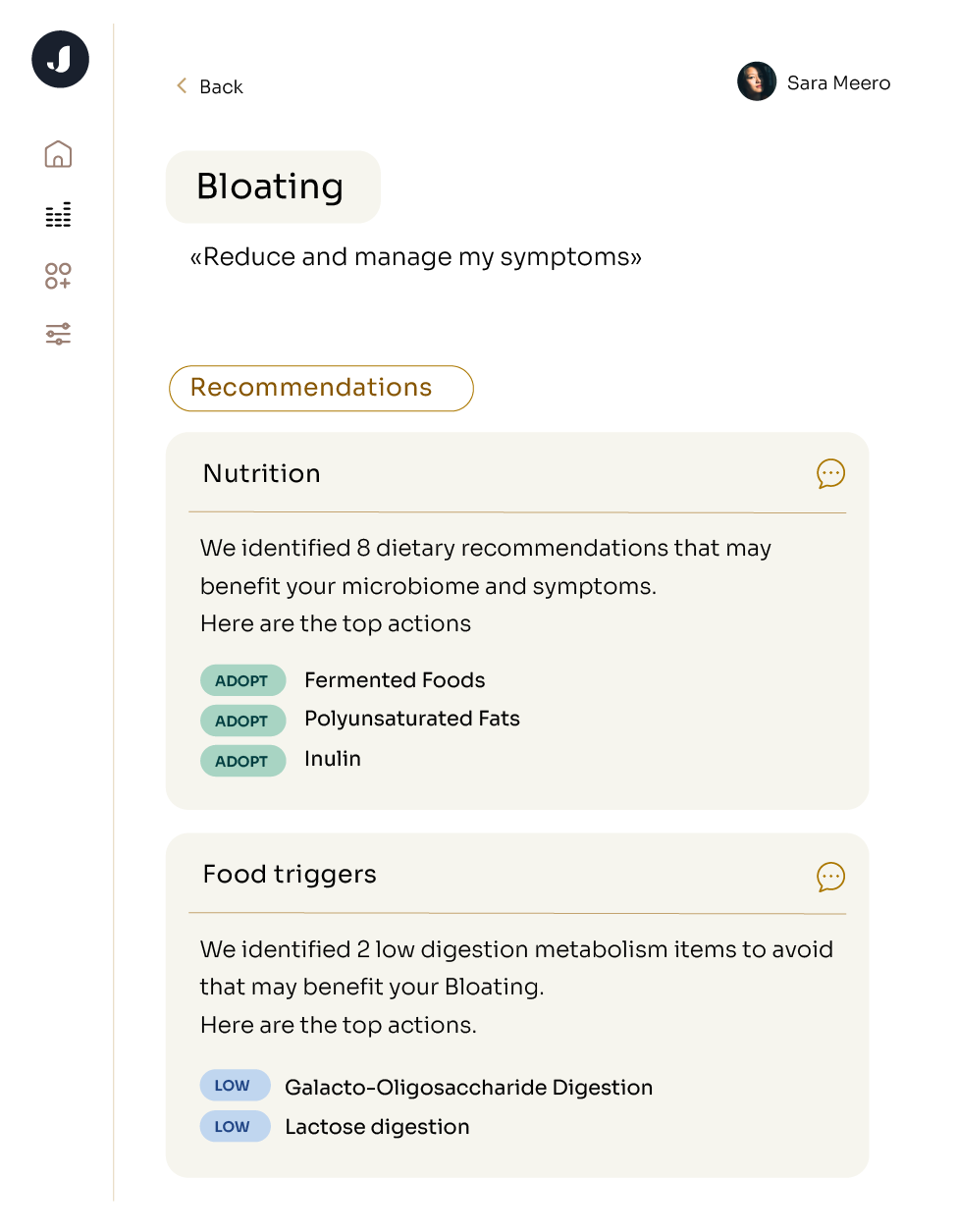
Eat A Healthy Diet
Eating a healthy and microbiome friendly diet is an essential tool for IBS management. Many foods like dairy and processed goods can exacerbate IBS symptoms. Other eating patterns such as the low-FODMAP diet could potentially be helpful for IBS, but longitudinal research fully evaluating the effect these diets have on our microbiome is lacking. See our blog post all about how to eat with IBS to learn more about foods to include or avoid.
- See Your Doctor About Treatment Plans
- Sometimes medications such as antispasmodics or antidiarrheals may be the best option to manage your symptoms. It is important to stay connected to a physician if you are living with IBS.
The Social Security Administration (SSA) has three criteria that build their strict definition of what a disability is:
- You cannot do work at the substantial gainful activity (SGA) level because of your medical condition.
- You cannot do work you did previously or adjust to other work because of your medical condition.
- Your condition has lasted or is expected to last for at least 1 year or to result in death.
Apart from these criteria, the SSA decides if you have a qualifying disability based on the answers to the following five questions:
- Are you working?
- Is your condition “severe”?
- Is your condition found in the list of disabling conditions?
- Can you do the work you did previously?
- Can you do any other type of work?
Visit the SSA website to learn more about the answers to these questions, special cases, or how you can qualify for benefits.
Deciding if IBS is a disability or not greatly depends on your definition of disability. Considering the SSA’s definition of total disability, IBS does not appear directly on the official list of disabling digestive conditions. This does not mean that it is impossible to receive benefits for IBS. It is still possible to receive benefits for IBS if it is proven to be as severe as another condition on that list, or if it does not allow you to work at the SGA level.
The Center for Disease Control (CDC) defines disability as follows: “A disability is any condition of the body or mind (impairment) that makes it more difficult for the person with the condition to do certain activities (activity limitation) and interact with the world around them (participation restrictions).” By this definition, the status of IBS as a disability is determined by how it affects your life and if it prevents you from participating in activities.
Because of variance in definition and individual experience, the question of if IBS is a disability cannot be answered with a simple yes or no, but requires careful consideration of individual circumstances.