Understanding IBS
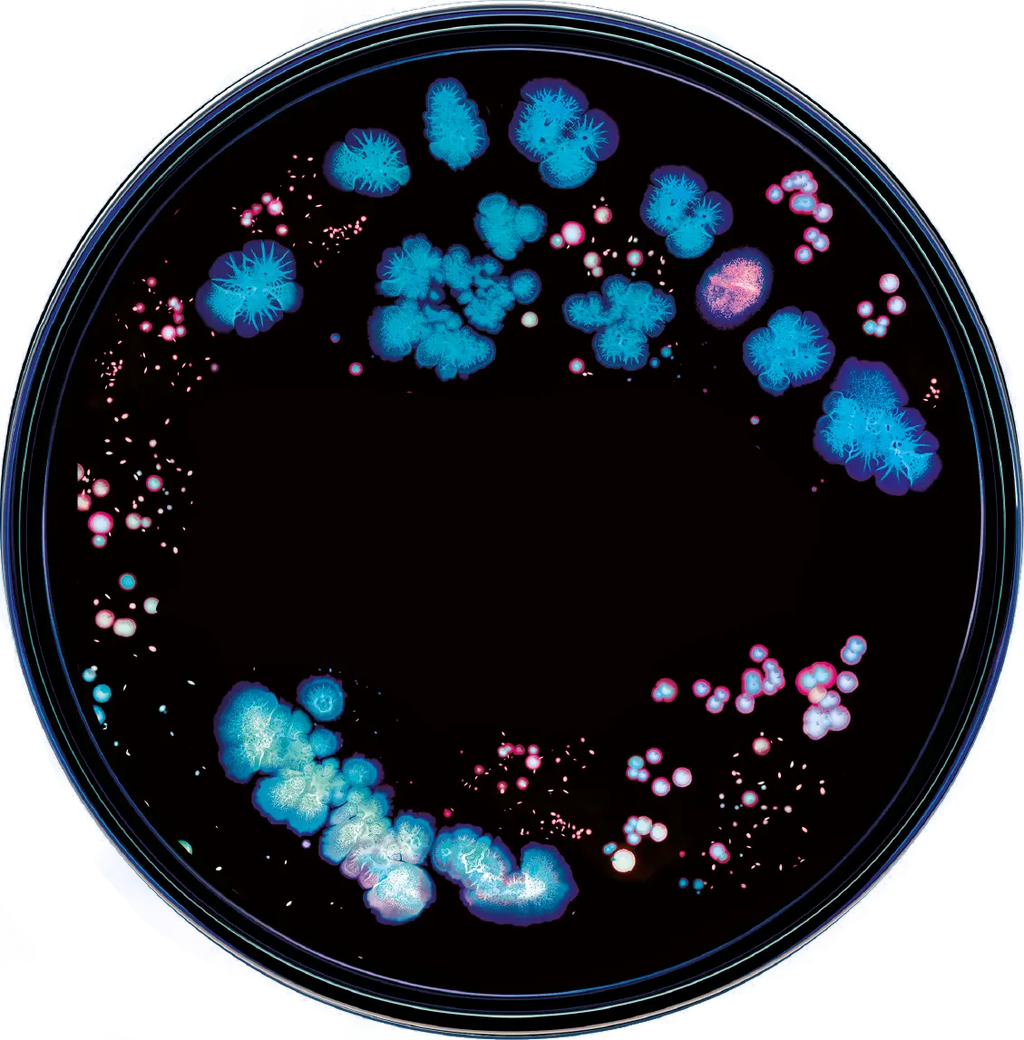
IBS is a complex and multifaceted condition. While its exact cause is not fully understood, it is believed to result from a combination of factors, including genetics, diet, lifestyle, and alterations in the gut microbiome. The gut microbiome, a community of microorganisms living in our intestines, plays a crucial role in digestion and overall health. Dysregulation of this microbiome can contribute to IBS symptoms. Individuals with IBS have been found to have decreased levels of beneficial bacteria like bifidobacterium and Faecalibacterium. Beneficial bacteria like these help their host digest foods like complex carbohydrates and fibers and are vital producers of short-chain fatty acids such as butyrate. These acids help strengthen the intestinal barrier and reduce inflammation in the colon. Microbes like these also protect the gut by competing for physical space, preventing harmful bacteria from taking hold in our gastrointestinal tract. IBS has also been associated with increased gut levels of potentially pathogenic bacteria such as Escherichia/Shigella. Certain strains of bacteria can produce toxins that can exacerbate symptoms of IBS.
Types of IBS
IBS is often classified into four main subtypes based on predominant symptoms. Some of these subtypes have been associated by research with further dysbiosis, or alteration of gut microbiota.
-
IBS-D (Diarrhea-Predominant): Characterized by frequent diarrhea, urgency, and loose stools. IBS-D has been linked to increased abundance of hydrogen sulfide producing bacteria such as Fusobacterium and Desulfovibrio. An overproduction of this gas can lead to irritation and diarrhea.
-
IBS-C (Constipation-Predominant): Marked by infrequent bowel movements, straining, and hard stools. Some studies have linked IBS-C to an increased level of methane producing bacteria such as Methanobrevibacter smithii, also called methanogens. An overabundance of these bacteria can lead to overproduction of methane from hydrogen sulfide and subsequent loss of gut motility.
- IBS-M (Mixed) and IBS-U (Unsubtyped): Involves a combination of diarrhea and constipation and when symptoms do not fit into any of the above categories respectively. These subtypes are not as well studied or easily characterized by their microbiome composition as the two types previously mentioned. Research into IBS-M and IBS-U is ongoing and evolving every day.
Recognizing which subtype you fall into is essential for understanding your condition and tailoring your management approach effectively.
Identifying an Attack
The first step to treating an IBS attack is recognizing it. An IBS attack, also called a flare-up, is a distressing episode characterized by a sudden onset of gastrointestinal symptoms that can vary in nature and severity. During an IBS attack, individuals often experience abdominal discomfort or pain, which can range from mild to intense cramping that may or may not be relieved by a bowel movement. The key hallmark of an attack is a disruption in bowel habits, leading to either diarrhea, constipation, or a fluctuation between both. This unpredictable shift in bowel movements can be accompanied by urgent or frequent trips to the restroom, causing significant inconvenience and discomfort. Bloating and excessive gas are also common during an IBS attack, contributing to the overall discomfort. If you are experiencing increased severity or frequency of symptoms, you may be suffering from an IBS flare-up.
Triggers
Once you’ve identified a flare-up, it is vital to identify your triggers that might have caused or worsened your symptoms. Common triggers for IBS symptom flare-ups are certain foods or dietary compounds like gluten. FODMAP foods, including fermentable oligosaccharides, disaccharides, monosaccharides, and polyols have also been implicated as triggers for IBS. Other common triggers for IBS are stress and anxiety, hormonal changes, environmental changes, and changes in medication. Another potential reason behind your IBS attack is changes in your microbiome that can result from a multitude of lifestyle factors. While the causal relationship between the microbiome and IBS symptoms is not fully understood, it can be an important factor to consider while identifying the causes of your flare.
Management Strategies
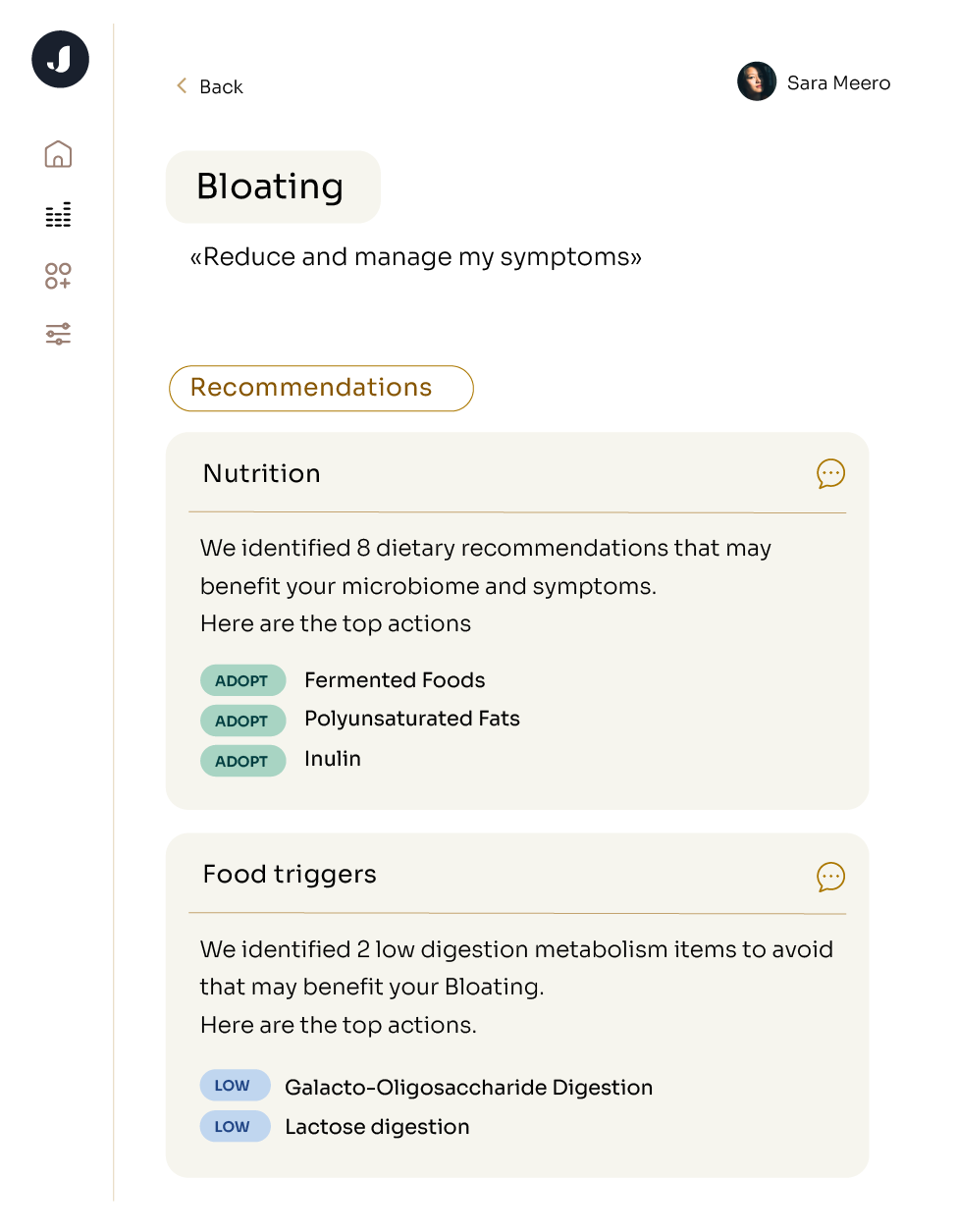
If preventative measures don’t stop your IBS attack, there are things you can do to reduce or manage the symptoms. Many of the following strategies, including diet and exercise, have been found to modulate the gut microbiome. Exploring what specific microbes are over or under abundant in your microbiome can help you to tailor your diet or exercise plans to target your IBS symptoms.
- Eating a healthy diet is a key component of managing IBS. Foods like high-fiber fruits and vegetables, lean proteins, whole grains, and probiotics can help reduce stomach troubles and improve digestion. Avoiding food triggers is one of the best diet-based strategies to manage IBS symptoms. Also, be sure to drink plenty of fluids – water is best – throughout the day as dehydration can worsen GI issues. Avoiding processed foods and sugary drinks can also help keep your gut balanced.
-
When it comes to exercise, try taking even just a few minutes each day for some gentle stretching or yoga poses, which can help release tension in your abdominal muscles and reduce stress. Although, be cautious when making changes to your exercise regime, as intense exercise can worsen or trigger IBS symptoms in some individuals.
-
Probiotics, which contain strains of healthy bacteria, may be able to restore the delicate balance of microorganisms in your gut. Some studies have provided evidence that multistrain probiotics containing Lactobacillus and Enterococcus can help alleviate symptoms of an IBS attack.
- Consult your doctor. If lifestyle changes, targeted microbiome treatments, or over-the-counter remedies do not provide relief, consult your healthcare provider. They may prescribe medications like antispasmodics, antidiarrheals, and medications that affect gut motility or recommend an alternative therapy such as cognitive behavioral therapy which has shown promise in managing IBS in individuals with stress and anxiety.