What is gluten and gluten sensitivity?
Gluten is a protein found in grains including wheat, barley, and rye (source). It’s what gives bread its pocketed texture and its chewiness. For many people, gluten can also be the source of digestive problems, such as bloating, pain, brain fog, migraines, constipation, or diarrhea (source). It’s found in bread products and beer and is also used as a thickener, so it can hide in soups, sauces, packaged food, and even in non-food items like Play-Doh (source).
Gluten has particular amino acid residues that are difficult for human enzymes to break down (source). In fact, there are many common, healthy foods that our enzymes can’t digest on their own and for which we depend on our microbiome to help digest. When you eat gluten, it is partially broken down by stomach acids and enzymes, and the remaining stubborn protein residues continue through the GI tract (source). For those without gluten sensitivity, these residues pass with no trouble. For others with gluten sensitivities, this undigested gluten can cause discomfort or even trigger reactions that damage your small intestine.
Gluten & Your Microbiome
The microbes in your gut are an important part of your digestive system. You have enzymes throughout your digestive tract that begin breaking down your food as soon as you start chewing it, but once food reaches the large intestine, your body relies on microbes to help finish the job.
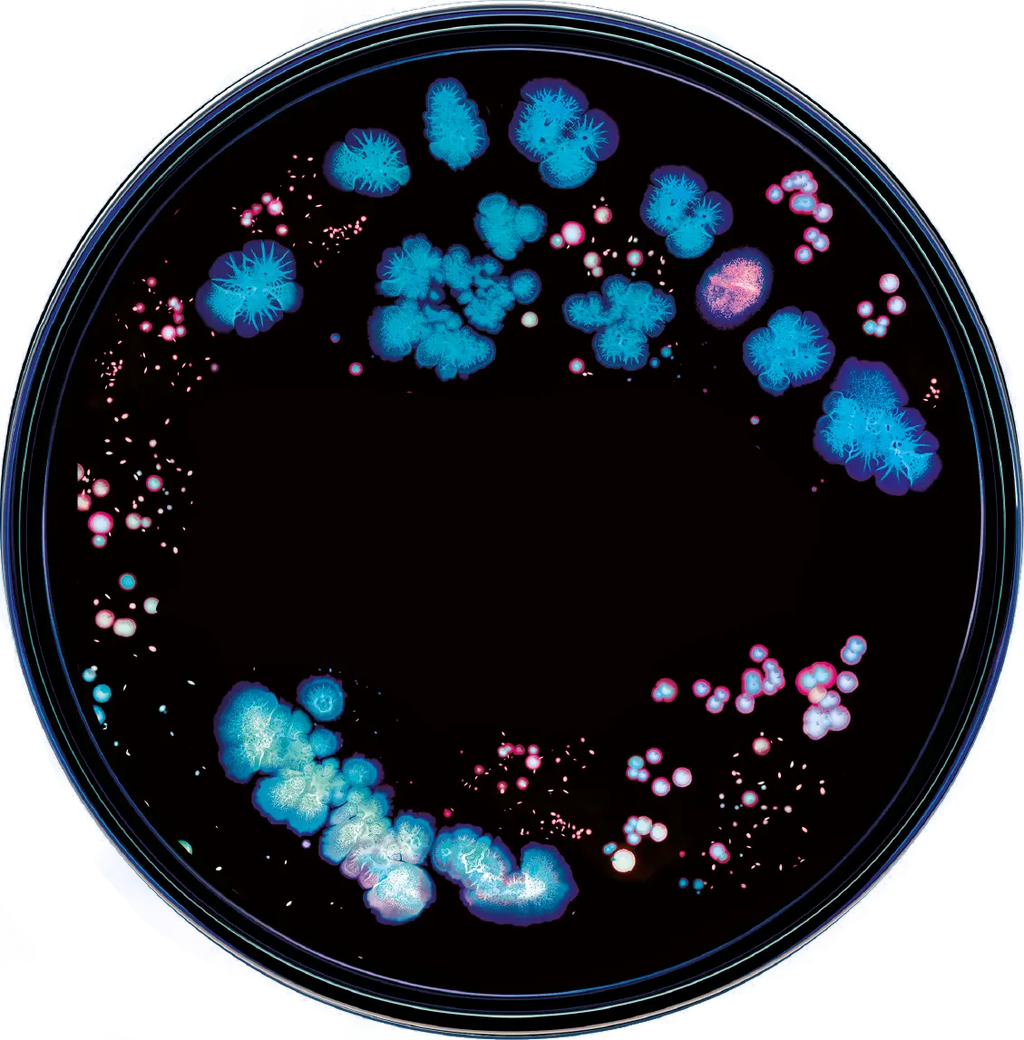
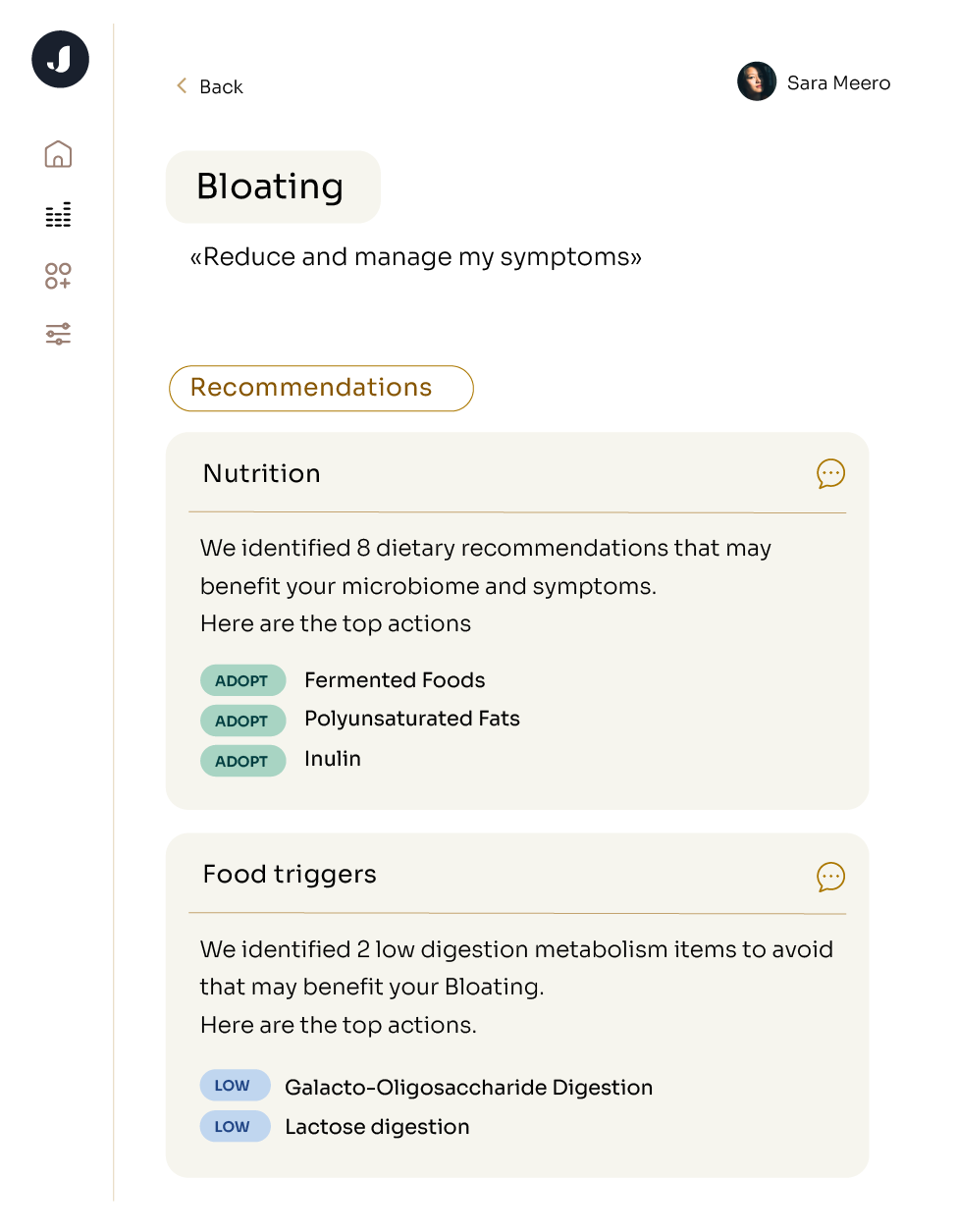
The gut microbiome may be involved with gluten intolerance, as some evidence shows that the gut microbiota can be altered in individuals with celiac disease and other types of gluten sensitivity (source, source). Most of the evidence regarding which bacteria can digest gluten comes from in vitro studies. This means that they’re done in Petri dishes, not in the body, as the gut environment is too crowded and complex to observe these processes. Studies show that gut microbes such as B. subtilis can degrade gluten residues when grown in Petri dishes (source), and researchers are still investigating the behavior of these microbes in the human body. To give you a full view of your gut’s digestive power, you’ll find these microbes mapped back to your personal gut microbiome in the Metabolisms section of your Jona Report.
What types of gluten intolerance exist?
There are several kinds of gluten intolerance with different symptoms, risks, and treatment. We’ll cover the three most common types: celiac disease, wheat allergy, and non-celiac gluten sensitivity (NCGS.)
Celiac Disease
Celiac disease (CD) is an autoimmune condition largely affecting the small intestine. The walls of a healthy small intestine are covered in tiny finger-like cells called villi, which create a large surface area to absorb nutrients. When a person with CD eats gluten, their body creates antibodies that attack and damage these villi, which reduces their ability to process any nutrients, not just gluten (source). Left untreated, individuals with CD can develop nutrient deficiencies, other autoimmune conditions, and even have an increased risk for some cancers (source). Early diagnosis for celiac disease helps to mitigate symptoms before they get worse, but this isn’t always in childhood - adults can develop celiac disease, too (source).
Unlike other conditions we’ll discuss here, celiac disease runs in families. Having a close relative with celiac disease puts you at roughly a 10% risk of also developing the condition as compared to about 1% if you have no relatives with the condition (source).
What will help me feel better?
There’s a lot of exciting research on the potential for manipulating the microbiome to improve celiac disease, but for now, the best treatment is to avoid gluten altogether (source).
Wheat Allergy
A wheat allergy is a serious reaction to wheat in any form. In these individuals, exposure can trigger anaphylaxis, headache, nausea and vomiting, and they may need to go to the emergency room (source).
What will help me feel better?
Children under the age of 12 may grow out of a wheat allergy. The Cleveland Clinic estimates that there’s about a ⅔ chance the allergy resolves itself in adulthood (source). However, if you’re an adult managing a wheat allergy, you need to avoid wheat at all costs, and carrying epinephrine (like an Epi-Pen, an injectable drug that constricts your veins to reduce the severity of an allergic reaction) can also be a good idea in the event of exposure.
Gluten Intolerance (aka Non-Celiac Gluten Sensitivity, NCGS)
Non-celiac gluten sensitivity is exactly what it sounds like: the presence of symptoms after gluten consumption in the absence of celiac disease or wheat allergy (source). Hypotheses abound as to the exact mechanisms behind this phenomenon (source, source), and more research is needed to define this diagnosis (source). You might have NCGS if you have ruled out celiac disease or a wheat allergy via medical testing but still have discomfort or symptoms when you eat gluten.
What will help me feel better?
Since there's no clear agreement on how to diagnose NCGS, there are also conflicting approaches to managing it. One study found that symptom severity in NCGS patients was unchanged when consuming gluten vs. a placebo (source), while others indicated that avoiding gluten and adopting a diet low in FODMAPs (fermentable oligo-, di-, and monosaccharides and polyols) improved symptoms in an NCGS cohort (source, source). (For more information on FODMAPs, check out our blog post.) Speaking with your doctor and a dietician, tracking how you feel after eating certain foods, and profiling your microbiome with Jona can all be good starting points for managing NCGS.